
Objetive: DEAR STUDENTS THE OBJETIVE OF THIS TRAINING , IS GIVE
YOU A BASIC UNDERSTANDIG OF PERITONEAL DIALYSIS PROCEDURE AND
ALLOW TO PROVIDE TO LEARNING ABOUT THE CHRONIC RENAL FAILURE
PATIENTS . WE ARE SURE THAT THE OBJECTIVES OF THIS TRAINING WILL
BE ACHIEVED. PROFESSORS…… 1
Chronic Kidney Failure Chronic kidney failure, also called
chronic kidney disease, describes the gradual loss of kidney
function. Your kidneys filter wastes and excess fluids from your
blood, which are then excreted in your urine. When chronic kidney
failure reaches an advanced stage, dangerous levels of fluid,
electrolytes and wastes can accumulate in your body. 7.2.1 The
peritoneal membrane / P. Martin 2

Chronic Renal Failure Slow progressive renal disorder related to
nephron loss, occurring over months to years. In the initial
Stage, CKD non present symptoms . Culminates in End Stage Renal
Disease 3
Causes of Chronic Renal Failure: HIV positive (Asocieted
Nephrophaty ) HIVAN (Namibia) Diabetes Hypertension Renal
vascular disease (also vascular disease) Nephritis Pyelonephritis
& chronic UT I Polycystic kidney disease Renal Neoplasms
Analgesic nephropathy Immunological disorders: Lupus, Goodpasture
syndrome, Metabolic disorders: gout Nephrotic Syndrome ?primary
or secondary 7.2.1 The peritoneal membrane / P. Martin 4

7.2.1 The peritoneal membrane / P. Martin 5

Treatment Options SubPeritoneal Dialysis Hemodialysis Kidney
Transplant Conservative management 6
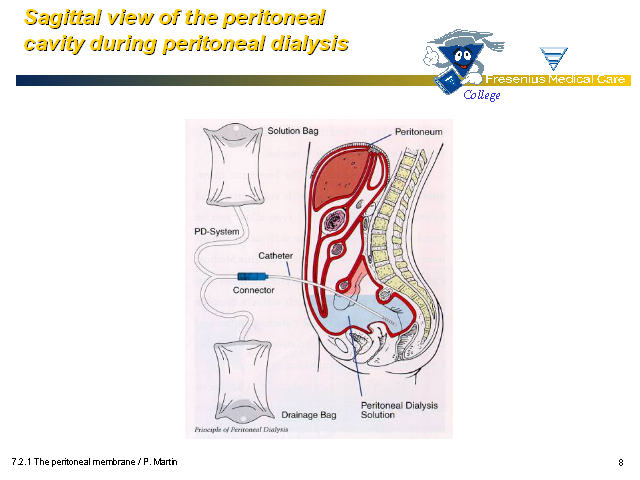
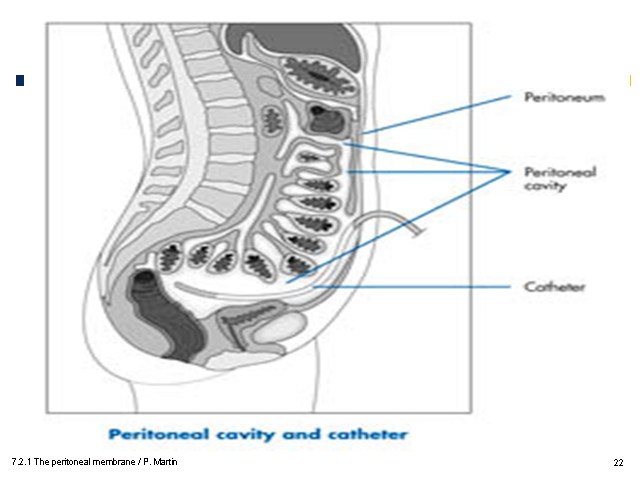
7.2.1 The peritoneal membrane / P. Martin 7 Sagittal view of the
peritonealcavity during peritoneal dialysis

7.2.1 The peritoneal membrane / P. Martin 8

7.2.1 The peritoneal membrane / P. Martin 9

10 The peritoneal anatomy A sagittal section trough the
peritoneal cavity General facts Living membrane Reusable Provides
lubrication for internal organs Normally contains 10 – 100 cc's
fluid Semipermeable Bi-directional

7.2.1 The peritoneal membrane / P. Martin 11 (Gp:) Transport
across the peritoneum (Gp:) Osmosis Diffusion Convection
Peritoneal physiology

7.2.1 The peritoneal membrane / P. Martin 12 Diffusion Peritoneal
physiology

7.2.1 The peritoneal membrane / P. Martin 13 RANDOM movement of
solutes across the peritoneal membrane from an area of high
concentration to an area of low concentration (without assistance
by any flow of fluid) Diffusion HIGH low Peritoneal
physiology

7.2.1 The peritoneal membrane / P. Martin 14 Factors affecting
diffusion solute size concentration gradient electrical charge
blood flow rates Peritoneal physiology

7.2.1 The peritoneal membrane / P. Martin 15 Movement of water
across the peritoneal membrane from an area of low concentration
to an area of high concentration. (Gp:) Osmosis low HIGH
Peritoneal physiology
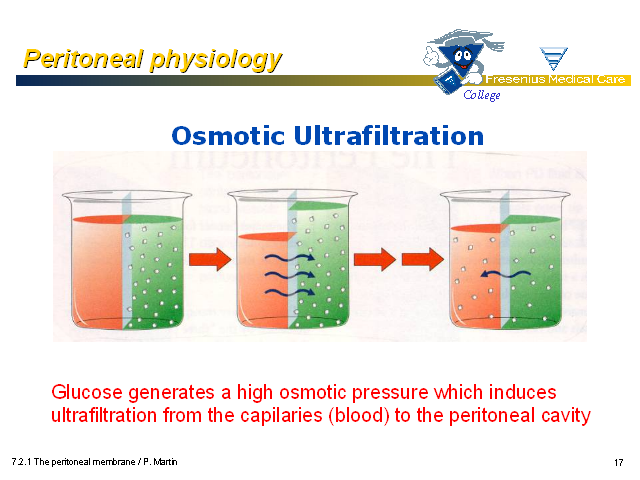
7.2.1 The peritoneal membrane / P. Martin 16 Osmotic
Ultrafiltration Peritoneal physiology Glucose generates a high
osmotic pressure which induces ultrafiltration from the
capilaries (blood) to the peritoneal cavity

7.2.1 The peritoneal membrane / P. Martin 17 Factors affecting
osmosis dextrose concentration dwell time membrane permeability
Peritoneal physiology

7.2.1 The peritoneal membrane / P. Martin 18 the dwell time the
peritoneum characteristics rapid transperitoneal absorption with
decline of the osmotic gradient in time: Dextrose 1.5%: maximum
UF rate of 9.27 mL/min Dextrose 4.25%: maximum UF rate of 21.0
mL/min Dextrose 1.5% removes 100-300 cc of extra water Dextrose
2.3% removes 300-500 cc of extra water Dextrose 4.25% removes
600-800 cc of extra water Fluid removal is dependent on:

7.2.1 The peritoneal membrane / P. Martin 19 Convection Solutes
move across the peritoneal membrane in an'orderly flow' from one
area to another by being carried by a flowing fluid. Peritoneal
physiology

7.2.1 The peritoneal membrane / P. Martin 20 Diffusion Convection
Ultrafiltration (osmotic pressure gradient) solute removal fluid
removal The composition of PD solution is the key factor that
governs diffusion, convection as well as the removal of fluid
excess from the body · Electrolytes correction ·
Body fluid balance · Acid-base control · Blood
purification Peritoneal dialysis
7.2.1 The peritoneal membrane / P. Martin 21

22

Peritoneal Dialysis Catheter Two double-cuff Tenckhoff peritoneal
catheters: standard (A), curled (B). 7.2.1 The peritoneal
membrane / P. Martin 23

Dialysis SubDialysis is the diffusion of solute molecules through
a semipermiable membrane, passing from higher concentration to
that of lower concentration. It is the process of separating
colloids and crystalline substances in solution by the difference
in their rate of diffusion through a semi permeable membrane. The
purpose of dialysis is to remove endogenous and exogenous toxins
and to maintain fluid electrolyte and acid- base balance till the
renal function recovers. It is a substitute for some excretory
functions of kidneys but does not replace the endocrine and
metabolic functions. 7.2.1 The peritoneal membrane / P. Martin
24

INDICATIONS Uremic symptoms with neurologic abnormalities
Persistent hyperkalemia, above 6.5 mEq/L Blood urea level more
than 50 mmol/l Serum Creatinine more than 900 µmol/l Severe
acidosis, pH less than 7.2, TCO2 less than 10-12 mEq/L
Hyperphosphatemia Pulmonary edema and CCF 7.2.1 The peritoneal
membrane / P. Martin 25
Peritoneal dialysis SubPeritoneal dialysis is a technique that
employs the patient’s peritoneal membrane as a dialyzer.
Excess body water is removed by an osmotic gradient created by
the high dextrose concentration in the dialysate; wastes are
removed by diffusion from the peritoneal capillaries into the
dialysate. Because peritoneal dialysis is not as efficient as
hemodialysis, it must be performed daily rather than 3 times
weekly as in hemodialysis. 7.2.1 The peritoneal membrane / P.
Martin 26

7.2.1 The peritoneal membrane / P. Martin 27

7.2.1 The peritoneal membrane / P. Martin 28

Phases of A Peritoneal Dialysis Exchange Fill: fluid infused into
peritoneal cavity Dwell: time fluid remains in peritoneal cavity
Drain: time fluid drains from peritoneal cavity 7.2.1 The
peritoneal membrane / P. Martin 29

7.2.1 The peritoneal membrane / P. Martin 30

INTERMITTEN PERITONEAL DIALYSISIPD (WILL DO IN IHO) 7.2.1 The
peritoneal membrane / P. Martin 31 WARD 7 NEW BUILDING

1.Continuous Ambulatory PD SubIt is the most commonly used method
of peritoneal dialysis. The filtration process occurs most hours
of the day. The exchange usually take about 3 minutes , 3-4 times
a day and only require a solution bag with tubing attached to it
that connects to the child’s blood stream. It gives
freedom. 7.2.1 The peritoneal membrane / P. Martin 32

2.Automated Peritoneal Dialysis Suba)Continuous Cyclic Peritoneal
Dialysis Continuous regimen means that the dialysis solution is
present in the peritoneal cavity continuously, with the exception
of short significant periods between exchange. It uses duel lumen
catheterization, i.e., 2 catheters, one for inflow and other for
outflow. 7.2.1 The peritoneal membrane / P. Martin 33

Intermittent Peritoneal Dialysis Sub-USUALLY DONE IN HOSPITAL It
means the dialysis sessions are performed several times a week.
This technique uses one catheter for inflow and outflow. Flow is
interrupted after both inflow and outflow during exchange. 7.2.1
The peritoneal membrane / P. Martin 34

PROCEDURE The abdomen is cleaned in preparation for surgery, and
a catheter is surgically inserted with one end in the
abdomen and the other protruding from the skin. Before each
infusion the catheter must be cleaned, and flow into and out of
the abdomen tested. The warmed solution is allowed to enter the
peritoneal cavity by gravity and remains a variable length of
time (usually 10-15 minutes) according to the rate of solute
removal and glucose absorption in individual patients. The total
volume is referred to as dwell while the fluid itself is
referred to as dialysate. 7.2.1 The peritoneal membrane / P.
Martin 35

SubThe dwell can be as much as 2.5 litres, and medication can
also be added to the fluid immediately before infusion. The
dwell remains in the abdomen and waste products diffuse across
the peritoneum from the underlying blood vessels. After a
variable period of time depending on the treatment (usually
4–6 hours), the fluid is removed and replaced with fresh
fluid. 7.2.1 The peritoneal membrane / P. Martin 36